 |
 |
 |
Vol.
23, No. 2
June 2018
The Impact of Opioids on the Child Welfare System
6 States Sue Maker of OxyContin as They Battle Expenses, Human Costs of Opioid Crisis
-- USA Today, May 15, 2018
Reversing the Deadly Opioid Crisis in NC
-- News & Observer, Feb 15, 2018
As recent headlines confirm, opioid misuse is a crisis for our state and our nation. Here in North Carolina, three people die from opioid overdose every day (NCDHHS, 2017). Deaths linked to opioids in NC grew by an astounding 900% between 1999 and 2016 (Worth & House, 2018). And as the figure below suggests, overdose deaths are just the tip of the iceberg.
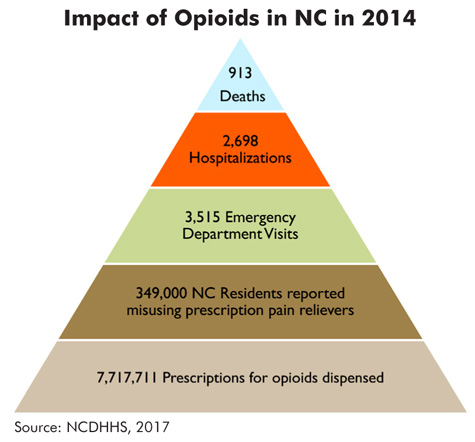
For every single opioid poisoning death in North Carolina in 2014, there were just under three hospitalizations, nearly four emergency department visits for medication or drug overdoses, over 380 people who misused prescription pain relievers, and almost 8,500 prescriptions dispensed for opioids (NCDHHS, 2017).
This epidemic has its roots in the heavy marketing of opioids and a well-intentioned but flawed emphasis on physicians' use of pain scales, which led to an increase in prescriptions for drugs like hydrocodone and oxycodone. By 2016, more than 675 million opioid prescriptions were dispensed in NC--more than 65 pills for each man, woman, and child in the state (Worth & House, 2018). This, along with the addictive potential of these drugs, led to an epidemic of drug addiction and overdose. In the last several years, the problem has worsened due to cheap and easy access to heroin, which sometimes contains the even more powerful drug fentanyl (Kansagra & Cohen, 2018).
Unintentional opioid-related overdose deaths are estimated to have cost North Carolina over $1.5 billion in 2015 (Kansagra & Cohen, 2018). By one estimate, the opioid epidemic has cost the U.S. more than $1 trillion since 2001 in lost wages and productivity, health care costs, reduced tax revenue, and increased spending on health care, social services, education, and criminal justice (Altarum, 2018).
What Is the Impact on the Child Welfare System?
But what about the impact on the child welfare system? For example, are opioids in some way behind the steady rise in the number of children in foster care in North Carolina and many other states?
A partial answer to this question comes from the Office of the Assistant Secretary for Planning and Evaluation (ASPE), which is part of the U.S. Department of Health and Human Services. In March 2018, ASPE issued two reports based on a study it conducted on the use of opioids and other substances and the child welfare system.
For the study, ASPE researchers used statistical models and administrative data to estimate the relationship between substance use and involvement with child welfare. They combined this quantitative information with interviews of 188 individuals from 25 U.S. counties, including counties hit hardest by substance abuse. Interviewees included child welfare administrators and practitioners, substance use treatment professionals, judges, and others.
Study results revealed a strong statistical relationship between two indicators of substance abuse (overdose death rates and drug-related hospitalization rates) and child welfare caseloads. (Although this study shows a relationship between substance use and child welfare caseloads, it does not prove causality.)
Specifically, researchers found a relationship between substance use and the following:
Higher Caseload Rates. Researchers found that indicators of substance abuse have a statistical relationship with child welfare caseloads. Even when socioeconomic and demographic traits are taken into account, counties with higher overdose death and drug hospitalization rates tend to have higher rates of CPS reports and substantiations.
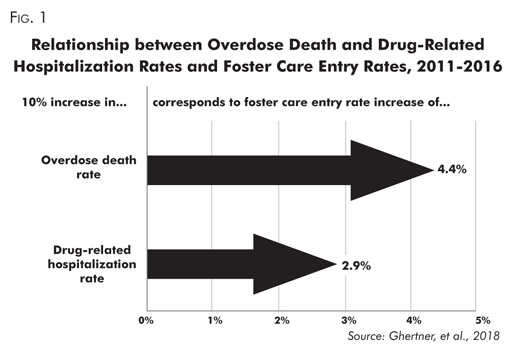
Higher Foster Care Entry Rates. Rates of drug overdose deaths and drug-related hospitalizations are also linked to higher rates of entry into foster care. This finding is illustrated in Figure 1, which shows a 10% rise in drug overdose death rates correlates with a 4.4% rise in foster care entry rates, while a 10% jump in drug-related hospitalizations correlates with 2.9% growth in foster care entry rates.
More Case Complexity & Severity. When indicators of substance use are high, child welfare cases are more likely to be more complex and/or severe, as measured by the proportion of maltreatment reports that are substantiated and by the proportion of children removed from their homes.
Interviews supported the link between substance use and case complexity. For example, researchers noted that "caseworkers and judges in areas hardest hit by the [opioid] epidemic described the difficulty of finding family to care for children because in many cases multiple members are misusing opioids. They described this as a substantial shift from recent years" (Ghertner, et al., 2018).
Other Findings
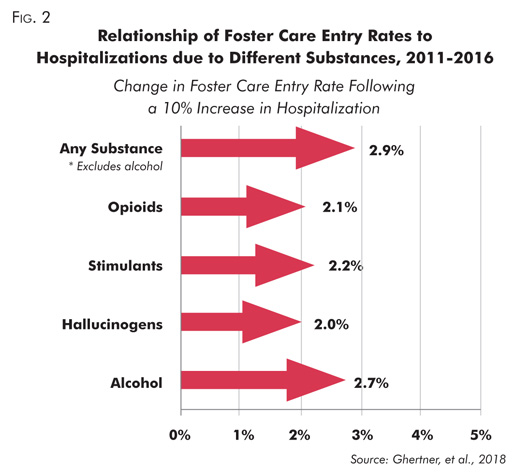
It's Not Just Opioids. A striking finding is that different substance types correlate in similar ways with foster care entry. Opioid-related hospitalization rates have a relationship with rates of entry into foster care comparable to that of other substance types, as Figure 2 shows. Note that alcohol has a stronger relationship with foster care entry than any illicit or prescription substance; alcohol-related hospitalizations are more than four times as prevalent as opioid hospitalizations (Radel, et al., 2018).
This Time Feels Different. Based on the study, Radel and colleagues conclude, "while the misuse of drugs has always been part of the constellation of issues affecting parenting in families involved in the child welfare system, the current [opioid] crisis has affected communities more broadly than past epidemics." Interviews revealed much pessimism about opportunities for family success. Many judges, lawyers, and court personnel were strongly inclined to favor placement when there is significant parental substance use, "often regardless of other factors" (Radel, et al., 2018).
Treatment Challenges. Researchers concluded a number of challenges are affecting how child welfare agencies and families interact with substance use treatment options, including lack of family-friendly treatment and misunderstanding and mistrust of medication assisted treatment (MAT). (Click here for more on MAT.)
Child Welfare Practice and Resource Issues. Interviews in the 25 U.S. counties participating in the study suggest that "child welfare agencies and their community partners are struggling to meet families' needs" (Radel, et al., 2018). For example, the system is wrestling with shortages of foster homes, inconsistent substance use assessment practices, and barriers to collaboration with substance use treatment providers and other stakeholders.
System Strengths. Researchers also acknowledged that across service systems, professionals recognized that "substance use disorders are chronic diseases, not simply moral failures," and noted the active efforts being made to secure more and better treatment options for parents (Radel, et al., 2018).
Read More. Follow the links below to read the original briefs on these studies:
- Substance Use, the Opioid Epidemic, and the Child Welfare System: Key Findings from a Mixed Methods Study, by Radel et al., 2018.
- The Relationship between Substance Use Indicators and Child Welfare Caseloads, by Ghertner et al., 2018.
Takeaways for Child Welfare Professionals
These reports confirm that child welfare agencies often feel the effects when communities struggle with substance use, and that the opioid epidemic seems to be having an unusually strong impact. These reports may prove useful to agencies explaining to others the challenges they face or justifying the need for additional resources.
The study is also confirmation that North Carolina is right to be taking steps to address the opioid epidemic. These include the state's Opioid Action Plan (see box below) and its efforts to improve recruitment of families for children in foster care.
Responses at the State and National Level |
While agencies try to assist families and cope with the expanding number of children in care, leaders at the national and state levels are also taking action. In October 2017, the White House declared the opioid epidemic a national public health emergency. In November, the president's commission on opioids released a lengthy set of recommendations, and in March 2018 the White House convened a summit on the opioid epidemic. The new Family First Prevention Services Act (H.R. 253) is also promising: although the effects will not be immediate, this law gives states more flexibility to spend federal money on critical services--including substance abuse treatment--that can prevent the need for foster care. In North Carolina, supported by a $31 million grant, the state has developed an Opioid Action Plan for the period 2017-21. The plan addresses seven core strategies:
For more on North Carolina's efforts, visit https://www.ncdhhs.gov/opioids It is hoped that these and future actions will have the desired effects. In the meantime, the need to find and sustain high quality resource families is more urgent than ever--a need our state's efforts around diligent recruitment and retention of resources families seeks to meet. Please see the June 2017 issue of Practice Notes for more on this effort. |